
September 3, 2024
Management Of Urinary Incontinence In Postmenopausal Females: An Emas Scientific Guide
Urine Incontinence An Overview You may be described a medical professional that specializes in urinary tract disorders (urologist) or a gynecologist with unique training in female bladder issues and urinary function (urogynecologist). Your medical professional may Biofeedback suggest that you do these workouts frequently to strengthen the muscles that help control peeing. Likewise referred to as Kegel exercises, these strategies are specifically reliable for stress and anxiety incontinence yet may likewise aid urge incontinence. Estrogen exhaustion is among the indicators of hormone inequality in women that is typically experienced during menopause. One of the most effective means to keep up with urinary system incontinence is via using grown-up baby diapers for women. A lot of females experience premenstrual syndrome (PMS) regarding 1-2 weeks prior to bleeding begins. An all natural technique that utilizes medicine, way of life adjustments, physical therapy, or various other interventions might help in reducing them or assist a person handle them. Lots of people believe that it's something that just goes along with aging and is an unavoidable concern. If you find that urinary incontinence is disturbing your daily activities and causing you to lose out on things you commonly enjoy, talk to your doctor.Hrt For Prostate Cancer Cells Patients
Genetic urinary system bladder hypoplasia might be a complement to ectopic ureters or other developmental disorders of the urinary system system. It most often influences the urinary system in individuals assigned woman at birth (AFAB). As many as 1 in 3 individuals who were AFAB will experience stress and anxiety urinary incontinence at some point.Reduced Estrogen Levels
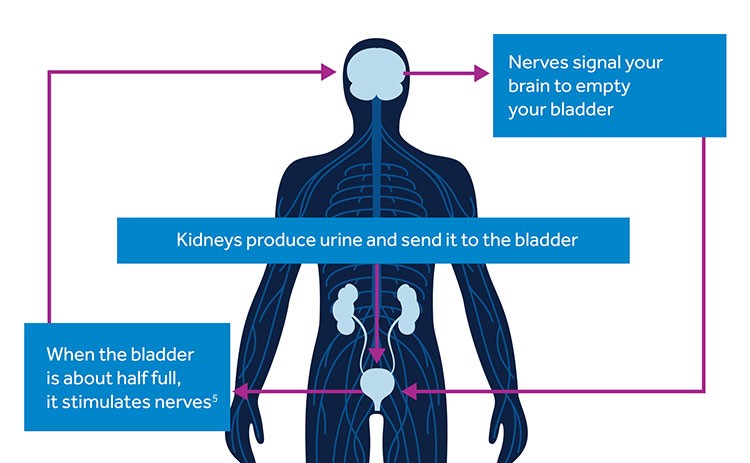
Your bladder resembles a storage tank-- once the bladder is complete, the brain sends a signal that it's time to urinate. Pee then leaves the bladder when a muscle mass opens (sphincter), allowing the urine to flow freely out of the body with the urethra. It is essential to determine the kind of urinary incontinence that you have, and your signs usually tell your physician which type you have. Throughout this process, the posterior wall of the urethra shears off the anterior urethral wall to open up the bladder neck when innate sphincter deficiency is present. Useful urinary incontinence is the failure to hold urine as a result of reasons besides neuro-urologic and reduced urinary system disorder. Videourodynamic research studies are reserved to review complex situations of anxiety urinary incontinence.- Ladies with severe inherent sphincter shortage do not always have the common urethral hypermobility throughout a Valsalva maneuver.
- Congenital malformations of the sacral spine can likewise create neurologic dysfunction leading to a flaccid, overdistended bladder with weak outflow resistance.
- Height was measuredto the nearby 0.1 centimeters utilizing a wall-mounted stadiometer.
- The research study consisted of 133 pre-menopausal females with normal durations that were not taking hormonal agents.
What hormonal agent maintains you from peeing?

Social Links