September 1, 2024
Result Of Conjugated Estrogen In Tension Urinary System Incontinence In Ladies With Menopause
Management Of Urinary System Incontinence In Postmenopausal Ladies: An Emas Clinical Overview [23] is titled the partnership in between menopause and urinary system incontinence that females with urinary system incontinence than those who did not have, dramatically had greater BMI [24] Medical care professionals should think about urinary incontinence a professional concern and create suitable diagnostic abilities. They must have the ability to determine and handle any kind of pertinent flexible aspects that might alleviate the problem.Drugs & Surgical Procedures
What hormone stops pee?
earn less pee during the night. Takeaway: If progesterone degrees are going up during and after your cycle, and progesterone triggers your bladder to get a lot more frequently, it may trigger urinary incontinence. Menstrual adjustments. There are many factors your month-to-month period can transform, however hormone inequality often plays a role.Hair problems.

Neurologic Causes
Your bladder is like a storage tank-- when the bladder is complete, the mind sends out a signal that it's time to urinate. Pee then leaves the bladder when a muscle mass opens (sphincter), enabling the urine to move freely out of the body with the urethra. It is very important to https://s3.eu-central-003.backblazeb2.com/5ghb9bmaj7etny/Vaginal-laxity/treatment/exploring-the-mental-impact-of-urinary739022.html figure out the type of urinary system incontinence that you have, and your symptoms frequently inform your physician which type you have. You might be described a medical professional that specializes in urinary system tract disorders (urologist) or a gynecologist with unique training in women bladder issues and urinary feature (urogynecologist). Your doctor may advise that you do these workouts frequently to reinforce the muscles that aid manage urination. Additionally referred to as Kegel workouts, these techniques are particularly efficient for tension urinary incontinence but may likewise assist urge urinary incontinence. Estrogen depletion is just one of the indicators of hormonal inequality in ladies that is usually experienced throughout menopause. One of the very best means to keep up with urinary incontinence is with using grown-up diapers for women. Your healthcare provider will carry out a physical exam (and a pelvic examination for people AFAB) and inquire about signs. You may need to keep a bladder journal for a couple of days to monitor your fluid intake, bathroom usage and pee leak. Your notes need to include what you were doing before the leak. Symptoms of overactive bladder or urge urinary incontinence in the lack of neurologic reasons are recognized merely as detrusor overactivity. Additionally, much study has actually been performed to reinforce the understanding of the neurophysiology of the bladder, urethra, and pelvic flooring. Finally, interest in the medical diagnosis and therapy of urinary incontinence is ongoing.- The urine then moves down through 2 slim tubes called the ureters.
- At 1 year, vital condition was understood for 99.9% of participants, including0.2% that were deceased and 0.1% that were shed to follow-up.
- The presence of inflammation in the bladder is believed to result in bladder muscle mass irritability and urge incontinence in some circumstances, as depicted in the picture below.
- Conflict exists regarding whether certain neurologic problems in patients with Parkinson illness lead to bladder disorder or if bladder signs and symptoms just relate to aging.
- An age-related pattern additionally shows up in the primary type of urinary incontinence experienced.
Find A Medical Test
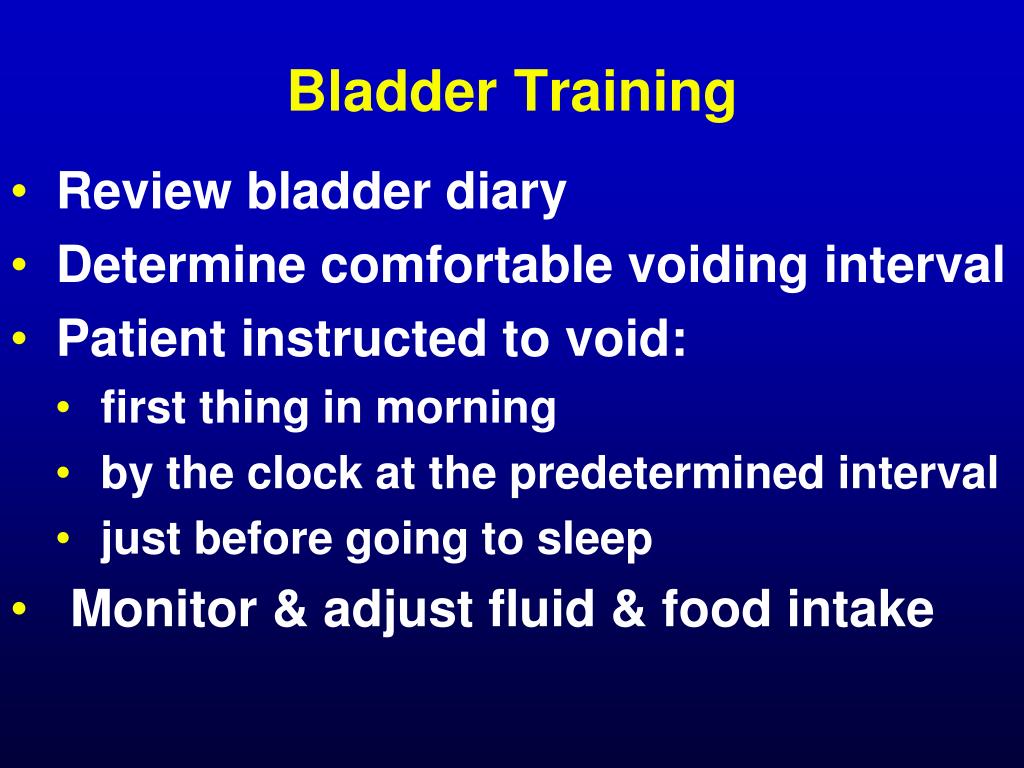
One of the treatments you may be suggested for taking care of UI is hormone treatment. Along with dealing with urinary incontinence, this therapy relieves several various other postmenopausal conditions, such as vaginal dryness, night sweats, and hot flashes. You can experience UI throughout your life, but the majority of episodes are the outcome of pressure or tension on the muscular tissues that aid you hold or pass pee. Hormonal agent adjustments can likewise influence your muscular tissue stamina in the pelvic area. For that reason, UI is extra typical in ladies who are expecting, giving birth, or going through menopause. The patient is trained to clear the bladder at a particular time of day. 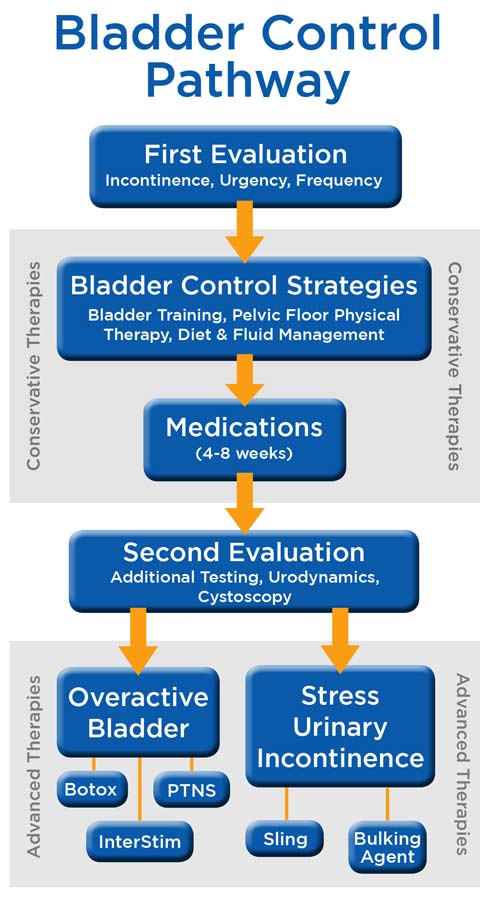
Social Links